WHAT IS NIPT TEST?
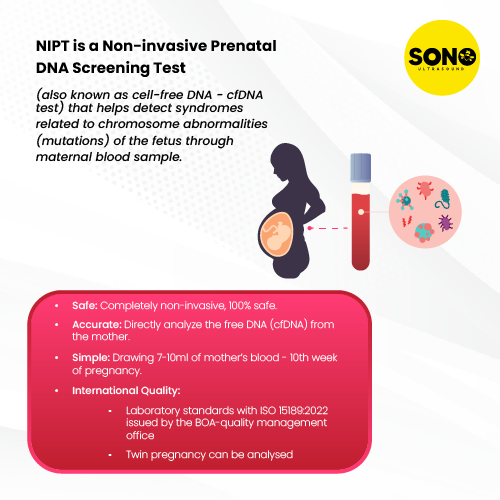
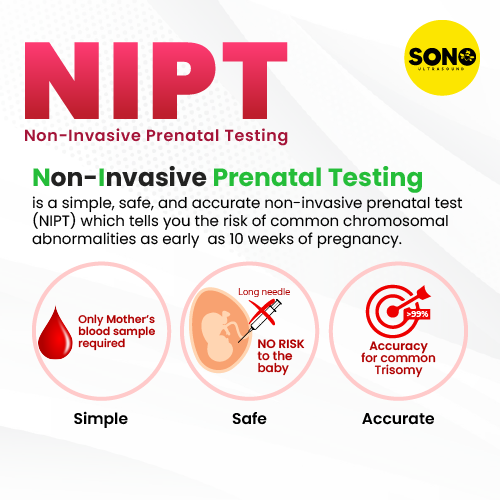
Non-invasive Prenatal Testing (NIPT) is a blood screening procedure performed on pregnant women to detect genetic disorders and abnormalities in the fetus. Although the test can be carried out as early as 10 weeks into pregnancy, it is recommended to be done from 12 weeks onwards.
WHY SHOULD YOU CONSIDER THE NIPT TEST?
While NIPT is a relatively expensive test, it is an excellent precautionary measure to identify potential health issues in the baby before birth. Genetic abnormalities like chromosomal trisomy, if left undetected, can cause serious physical, mental, and social challenges for the baby. For instance, Down syndrome (Trisomy 21) can lead to reduced mental capacity and visible deformations, while Patau’s syndrome (Trisomy 13) has extremely high death rates, with over 9 out of 10 children dying in their first year of life.
Being aware of potential dangers and consequences through preventive healthcare measures like detailed scans and NIPT gives families the time to prepare for the baby and possible conditions it may have. This preparation can include learning about the condition, developing treatment or therapy plans, and researching assistive technologies that can improve the baby’s day-to-day life.
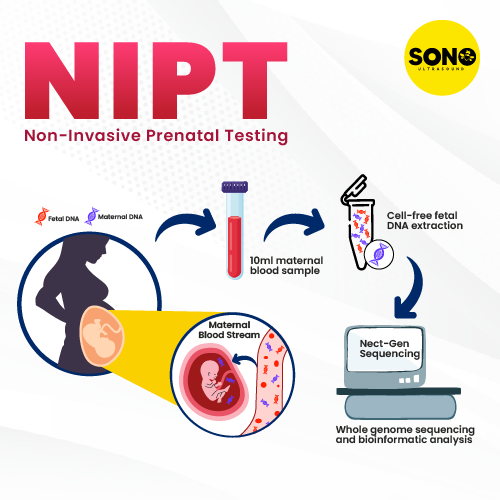
HOW DOES NIPT WORK?
A mother’s blood contains traces of the baby’s DNA, which can be used to sequence and analyze the genetic information of the fetus. The medical professional performing the test will extract blood from the mother’s arm using a needle and syringe and place it in a specific tube (cell-free DNA blood collection tube/BCT) to be sent off for analysis. The extraction process is similar to that of a typical blood withdrawal and is generally not painful.
The mother’s plasma contains the cell-free DNA (cfDNA) of the fetus, which is then sequenced to examine genetic information. The DNA of the baby is screened and analyzed from the mother’s blood sample.
WHAT CAN NIPT TEST FOR?
NIPT can be used to test for the following:
- Gender determination
- Chromosomal trisomy (three chromosomes rather than the normal pair of chromosomes)
- Down syndrome (Trisomy 21)
- Edwards syndrome (Trisomy 18)
- Patau’s syndrome (Trisomy 13)
- Sex chromosome trisomies (XXX, XXY, XYY)
- 22 types of fetal chromosomal aneuploidy (abnormal number of chromosomes)
- 20 types of microdeletion/microduplication syndromes (parts of the gene are duplicated or deleted)
WHY CHOOSE SONOBEE ULTRASOUND’S NIPT?
At SONOBEE ULTRASOUND, we use a modern and sensitive sequencing technique to screen for fetal aneuploidy that is highly specific and reflects the situation of abnormal chromosomes directly. The sequencing data is analyzed using an established bioinformatic pipeline with comprehensive databases, which ensures the use of reliable and detailed information sources. The results are calculated as a Z-score, which represents the quantitative variations of the chromosome of interest. This score is helpful for accurate judgment of NIPT results as it is significantly associated with true-positive results and has an excellent clinical association.
Our NIPT has been validated with clinical experience from over 140,000 pregnancies, which assures our clients of accurate results.
SENSITIVITY AND POSITIVE PREDICTIVE VALUE:
NIPT has a high sensitivity, which means that it can correctly identify patients with a disease. Additionally, the positive predictive value (PPV) measures the probability that they have the disease given a positive test result.
Get Your NIPT Testing Today!
Frequently Ask Questions about Non-Invasive Prenatal Testing (NIPT Test)
NIPT (Non-Invasive Prenatal Testing) is based on the analysis of fetal cell-free DNA present in maternal blood and does not rely on the biochemical markers of maternal blood. Therefore, pregnant women undergoing the test are NOT required to fast.
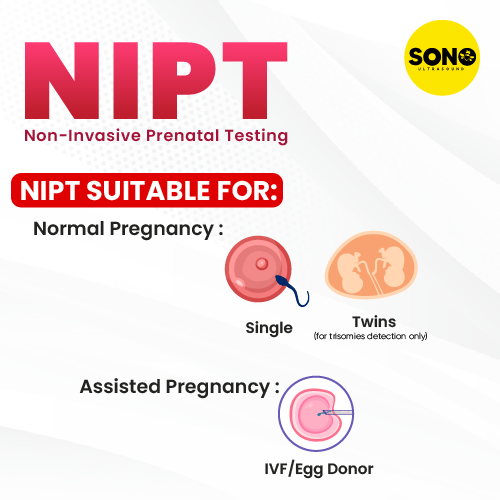
NIPT can be performed starting from the 10th week (10 weeks and 0 days) for naturally conceived pregnancies, and from the 8th week (8 weeks and 0 days from the date of embryo transfer) for IVF pregnancies. There is no gestational age limit, so it can still be conducted at 20 or 30 weeks. However, it is recommended that pregnant women undergo NIPT as early as possible. This allows doctors to promptly consider follow-up actions if any abnormalities are detected in the results.
If the pregnant woman had a blood transfusion in the past (e.g., 1-2 years ago), NIPT can be performed as usual. However, if the transfusion occurred within the last 6 months, foreign DNA from the donor may still be present, and NIPT is not recommended. If there is insufficient evidence to draw a conclusion during sample analysis, we will notify the patient to provide a new sample.
NIPT is a screening test for chromosomal abnormalities and certain microdeletions that can lead to common genetic syndromes in children. Currently, there is no scientific evidence suggesting that Hepatitis B (HBV), Hepatitis C (HCV), or Rubella affect the results of NIPT. However, NIPT remains a screening test, so routine ultrasound examinations and prenatal check-ups are still necessary to monitor for other potential issues.
There are currently no specific scientific studies confirming the effects of antiallergy medications on fetal development. However, potential risks of congenital abnormalities cannot be entirely ruled out. It is recommended that you consult a specialist for detailed advice, undergo regular prenatal check-ups, and have routine ultrasounds to monitor the baby’s development. You may also consider NIPT to screen for chromosomal abnormalities that can lead to conditions such as Down syndrome, Edwards syndrome, or Patau syndrome.
*Cleft lip and palate can result from both genetic and environmental factors.
- Genetic factors: NIPT can detect Patau syndrome and DiGeorge syndrome, both of which are associated with an increased risk of cleft lip or palate. However, not all babies with these syndromes will have cleft lip or palate.
- Environmental factors: Cleft lip and palate can also arise from non-genetic causes, such as environmental influences (e.g., smoking or the use of certain antiepileptic medications). Cleft lip and palate are multifactorial congenital defects. Without proper care, they can lead to challenges with feeding and speech. Babies born with these conditions often undergo corrective surgery early in life.
- Your baby’s test results are good.
- However, it’s important to note that no screening test worldwide can guarantee with 100% certainty that a baby is completely healthy. NIPT is a screening method that detects chromosomal abnormalities and certain microdeletions associated with common conditions such as Down syndrome, Edwards syndrome, and Patau syndrome. It is currently the most accurate screening test available, with up to 99.9% accuracy for detecting Down syndrome. That said, fetal development is influenced by many factors beyond what NIPT can detect. Therefore, even with normal NIPT results, it is still essential for pregnant women to attend regular prenatal check-ups and ultrasounds to monitor the baby’s development throughout the pregnancy.
During pregnancy, a certain amount of fetal DNA is released into the mother’s bloodstream, known as cell-free DNA (cfDNA). With advancements in science and the development of next-generation sequencing technology, American scientists have developed a method to analyze cfDNA for screening genetic conditions in the fetus using maternal blood, without the need for invasive procedures.
NIPT is a screening method for syndromes related to chromosomal abnormalities in number and structure; it does not screen for neural tube defects. Neural tube defects can be detected through the following methods:
- Ultrasound (at 18-22 weeks): Can detect up to 90% of neural tube defects.
- Triple Test (at 15-20 weeks): Can identify up to 70% of neural tube defects.
*Double Test is a screening test that uses biochemical markers such as free β-hCG and PAPP-A in the maternal blood, combined with factors like maternal age, weight, and height to assess the risk of certain syndromes such as Down syndrome, Edwards syndrome, and Patau syndrome.
+ Accuracy: Approximately 75%.
+ Timing: Performed in the first trimester (between 11 weeks + 1 day and 13 weeks
+ 6 days).
Often combined with a nuchal translucency ultrasound for more accurate results.
*Triple Test measures three markers: hCG, AFP, and estriol. These levels help calculate the risk of fetal abnormalities.
Best timing: Between 16-18 weeks of pregnancy (measuring maternal serum AFP, free β-hCG, and uE3, along with maternal age, weight, race, gestational age, and number of fetuses). Assesses the risk of Down syndrome, Edwards syndrome, Patau syndrome, and provides insights into neural tube defects. Ultrasound can also detect about 90% of neural tube defects.
+ Accuracy: About 50-60%.
+ Performed in the second trimester (between 14-22 weeks).
Both Double and Triple tests have lower accuracy with high false-positive and falsenegative rates.
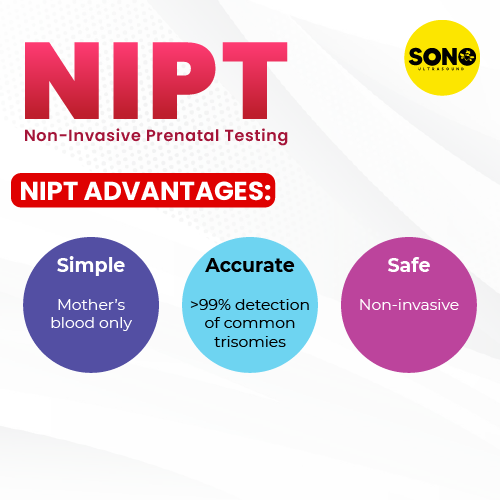
*NIPT (Non-Invasive Prenatal Testing) is a non-invasive screening method that analyzes fetal cfDNA in maternal blood to detect genetic disorders. The International Society for Prenatal Diagnosis (ISPD) recommends NIPT as the first-line screening for all pregnant women. Advantages of NIPT over Double/Triple Test:
1. No gestational age restrictions: Unlike Double Test (11-13 weeks) and Triple Test (16-18 weeks), NIPT can be performed from as early as 10 weeks.
2. Accuracy: NIPT is up to 99.9% accurate for detecting Down syndrome, as it analyzes fetal DNA from maternal blood and is not influenced by maternal factors such as age or ethnicity.
3. Clear results: NIPT provides a definitive “YES” or “NO” for detecting chromosomal abnormalities.
4. NIPT can be performed for single pregnancies, twin pregnancies, IVF pregnancies, surrogacy, and donor eggs.
Ultrasound assessment of nuchal translucency (NT) provides a relative estimation of the risk of Down syndrome in the fetus. However, it does not definitively confirm whether the baby has Down syndrome based solely on NT measurements and ultrasound findings. To obtain a certain diagnosis and appropriate guidance for the pregnancy, a combination of screening and diagnostic tests is required.
Although NIPT has a high accuracy rate of up to 99.9% for Down syndrome, it remains a screening test rather than a diagnostic one, and there is still a small falsepositive rate of approximately 0.012%. This may arise from factors related to placental development or maternal physiology.
Therefore, to confirm whether the fetus truly has abnormalities, additional diagnostic methods, such as amniocentesis or chorionic villus sampling (CVS), may be required (not attributable to the fetus). Thus, it is essential for the expectant mother to consult with her healthcare provider to monitor the pregnancy and receive guidance on undergoing diagnostic procedures like amniocentesis to reaffirm the results before making further decisions.
- NIPT is a test recommended by the International Society for Prenatal Diagnosis (ISPD) as the primary screening method for all pregnant women.
- During in vitro fertilization (IVF), only stable embryos that have the potential to develop are selected; however, this process does not assess whether these embryos have chromosomal abnormalities. Therefore, women undergoing IVF should also be screened with NIPT.
Preimplantation Genetic Testing (PGT) is a screening test for chromosomal abnormalities in embryos prior to transfer (typically at the 3-day or 5-day stage) or for diagnosing single-gene disorders such as thalassemia. This testing at this stage only assesses whether the 3-day or 5-day embryo is suitable for implantation in the uterus; it cannot ensure that the resulting child will be entirely normal.
Since PGT examines the embryo at an early stage, once the embryo is implanted in the mother’s uterus, numerous factors can influence its development and potentially lead to congenital anomalies. Non-Invasive Prenatal Testing (NIPT) is a screening method for chromosomal abnormalities in the fetus after it has formed. Therefore, reevaluating through NIPT is extremely important for couples undergoing IVF, regardless of whether they have performed PGT.
- The mother has received a blood transfusion or stem cell transplant within the last six months (as foreign DNA may still persist in the mother’s body).
- The gestational age is insufficient (from 10 weeks 0 days for natural conception; from 8 weeks 0 days for IVF, calculated from the date of 5 day embryo transfer).
- It is important to consider whether the fever is a common one or indicative of a potential malignancy.
+ Common fever (due to a cold or viral infection) => Refer to question 43.
+ Fever associated with cancer
“For breast cancer, lymphoma, and leiomyosarcoma, the size and extent of the tumor may alter the success rates of complete surgical resection and potentially change the type of additional chemotherapy and/or radiation therapy that is recommended. For those women diagnosed with leukemia or myeloma, it is less likely that the timing of diagnosis will alter treatment decisions.
However, these latter two malignancies often result in non specific symptoms (e.g., fevers, infections) that could easily be confused with other non-malignant disorders. A cancer diagnosis in 7 out of 49 cases with multiple aneuploidies is significantly higher than the majority of cancer screening tests currently in use. As opposed to Dr. Bianchi’s description, I would argue that these data strongly suggest that for NIPT results indicating multiple aneuploidies (1 in 10,000 NIPT cases), the test report should note that it is suggestive of concurrent maternal malignancy and provide the pregnant woman and her physician with an estimate of the detection rate and the possibility of a false positive result.”
Currently, there are no scientific articles or evidence confirming that maternal viral infections impact the results of NIPT. Women infected with hepatitis B, C, or HIV are encouraged to undergo non-invasive prenatal screening.




Reviews
There are no reviews yet.