A nuchal fold scan, also known as a Nuchal Translucency (NT) scan, is an early pregnancy ultrasound performed between 11 and 14 weeks to measure the fluid-filled space at the back of the fetus’s neck. An increased measurement can indicate a higher risk for certain chromosomal abnormalities, such as Down syndrome, as well as other genetic disorders and some heart defects. It is a non-invasive procedure that provides information for parents and doctors to consider, and it is often combined with a maternal blood test for a more accurate risk assessment.
The journey of pregnancy is filled with moments of joy, anticipation, and, understandably, a degree of anxiety. As you navigate your prenatal care, you’ll encounter a series of tests and scans designed to monitor your baby’s health and development. One of the first major screening tests offered is this very Nuchal Fold Scan.
This article serves as your in-depth guide to understanding this important prenatal procedure. We will explore what it is, what to expect, and how to interpret the results, empowering you with knowledge for this significant step in your pregnancy.
What is a Nuchal Fold Scan?
A Nuchal Fold Scan, more accurately called a Nuchal Translucency (NT) Scan, is a specialized ultrasound examination performed during the first trimester of pregnancy. Its primary purpose is to assess your baby’s risk for certain chromosomal abnormalities, most notably Down syndrome (Trisomy 21), as well as Edwards syndrome (Trisomy 18) and Patau syndrome (Trisomy 13).
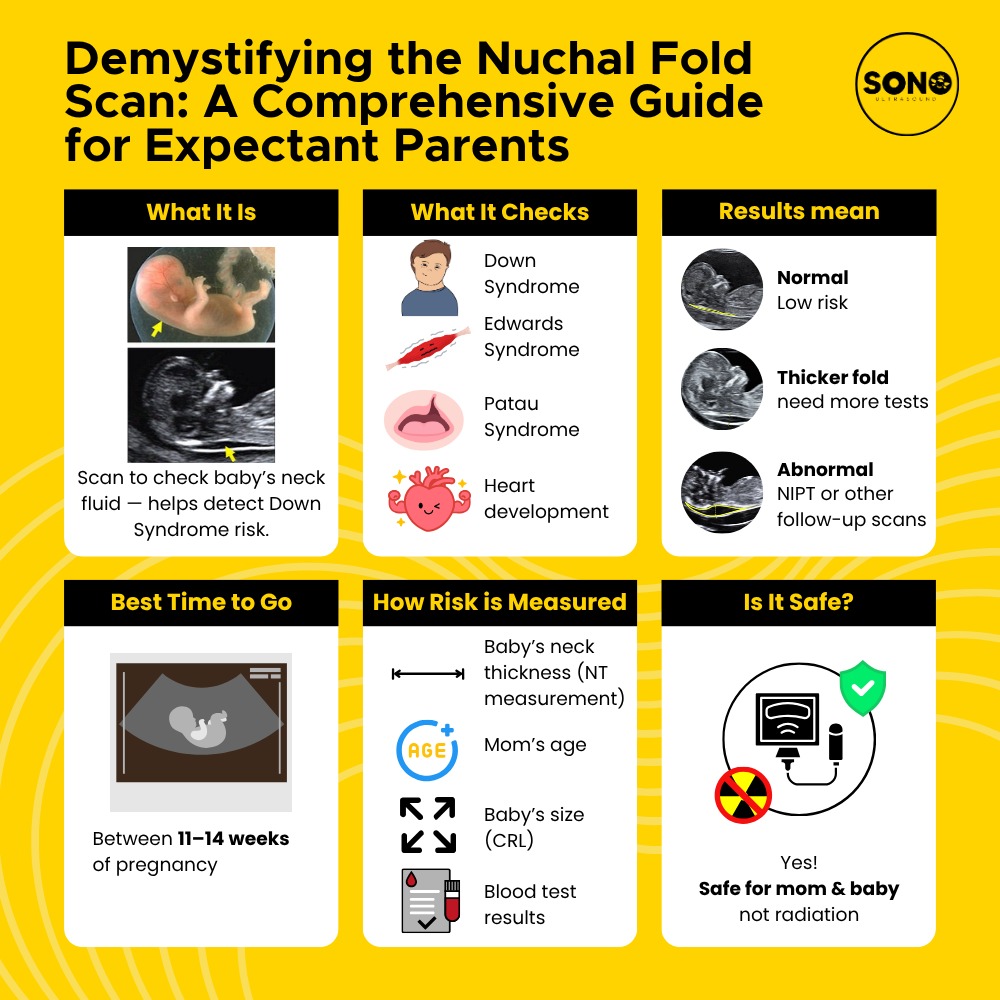
The term “nuchal translucency” refers to the small, fluid-filled space at the back of a developing baby’s neck. All babies have some fluid in this area, but research has shown that babies with chromosomal abnormalities tend to accumulate more fluid, leading to a larger-than-average measurement. The NT scan uses high-resolution ultrasound to precisely measure this translucent space.
It is crucial to understand what this test is—and what it is not.
- It is a Screening Test: The NT scan is not a diagnostic test. This means it cannot tell you for certain if your baby has a condition. Instead, it calculates the statistical probability or risk of an abnormality being present. It’s like a sophisticated red flag that helps identify pregnancies that might benefit from further, more invasive diagnostic testing.
- It’s Part of a Combined Screening: The scan is most effective when combined with blood tests that measure levels of certain pregnancy-associated hormones (Pregnancy-Associated Plasma Protein-A and human Chorionic Gonadotropin, or hCG). Together, the NT measurement and the bloodwork form the First-Trimester Combined Screening Test, which provides a more accurate risk assessment than either component alone.
When is the Right Time to Do an NT Scan?
Timing is absolutely critical for the NT scan. It must be performed during a very specific window in your pregnancy:
- Between 11 weeks and 13 weeks plus 6 days of gestation.
- When your baby’s crown-rump length (CRL) measures between 45mm and 84mm.
Why is the timing so precise? Before 11 weeks, the baby is too small to obtain an accurate measurement. After 14 weeks, the lymphatic system develops, and the excess fluid is naturally absorbed, making the nuchal translucency measurement unreliable. Adhering to this narrow timeframe ensures the results are valid and meaningful.
What to Expect During the Procedure
The NT scan is a straightforward and non-invasive procedure that feels very similar to a standard ultrasound.
- Preparation: Typically, no special preparation is needed. Some clinics might suggest you drink a few glasses of water before your appointment and avoid emptying your bladder, as a full bladder can sometimes help tilt the uterus into a better position for imaging. However, with modern ultrasound technology, this is less critical than it used to be.
- The Process: You will lie on an examination table, and a sonographer will apply a warm, water-based gel to your abdomen. They will then use a handheld device called a transducer, gliding it over your belly to capture images of your baby. In some cases, if your uterus is tilted or if you have a higher body mass index (BMI), a transvaginal scan (where a probe is inserted into the vagina) might be necessary for a clearer view. This is safe and generally not uncomfortable.
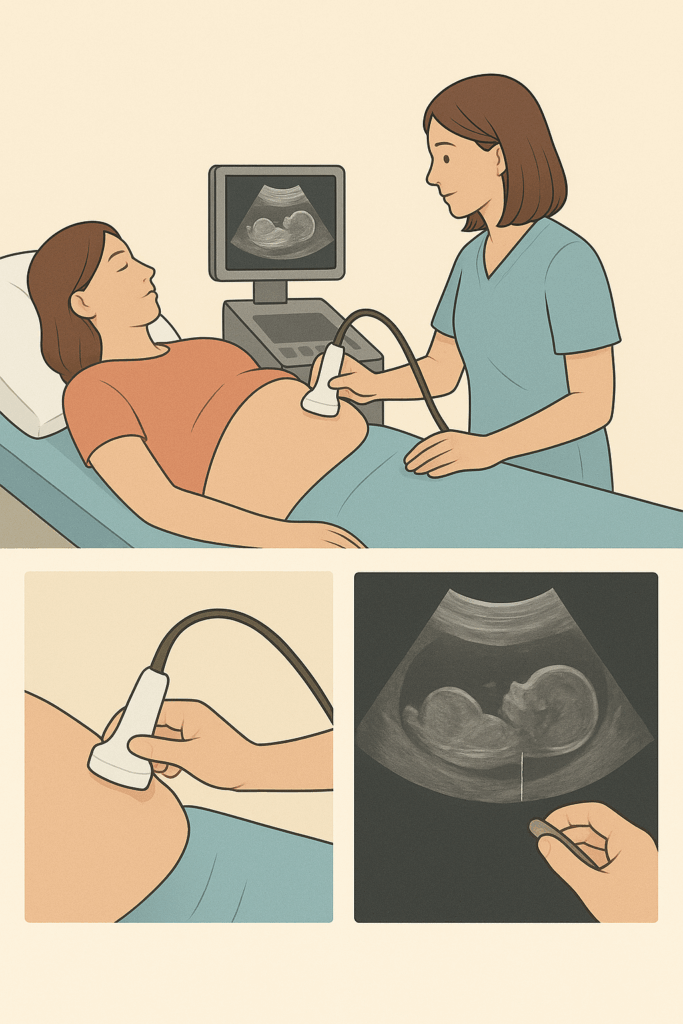
3. The Measurement: The sonographer will take various standard measurements to confirm your baby’s due date. Then, they will focus on obtaining a perfect profile view of the baby. They will magnify the image and carefully measure the nuchal translucency—the black (fluid-filled) space between the white lines of the baby’s skin and the underlying tissue. They may take several measurements to ensure accuracy. The entire process usually takes between 20 to 40 minutes.
What Do Your NT Scan Results Mean?
You will typically receive your results in the form of a “risk assessment.” This is not a simple “positive” or “negative.”
- The Measurement: The sonographer will record the NT measurement in millimeters. In a typical pregnancy, the nuchal translucency measurement is usually less than 2.5mm. A larger measurement indicates an increased risk of chromosomal abnormalities.
- The Risk Ratio: Your results will be presented as a ratio (e.g., 1 in 1,200 or 1 in 150). This number represents the calculated chance that your baby has a chromosomal condition. For example, a result of “1 in 1,200” means that for every 1,200 women with this same result, one is likely to have a baby with Down syndrome. Conversely, a result of “1 in 150” indicates a higher risk.
A “screen negative” or “low-risk” result means the chance of your baby having a chromosomal abnormality is very low, and no further action is typically recommended. A “screen positive” or “high-risk” result means the chance is high enough to warrant discussing further diagnostic options with your doctor or a genetic counselor.
What Happens if an NT Scan Is Abnormal?

Receiving a “high-risk” or “screen positive” result can be concerning, but it is vital to remember that this is a screening, not a diagnosis. Many women with an abnormal NT scan go on to have perfectly healthy babies.
Your healthcare provider will discuss the next steps, which usually involve seeing a maternal-fetal medicine specialist or a genetic counselor. They may recommend diagnostic tests to get a definitive answer. These include:
- Chorionic Villus Sampling (CVS): Can be performed between 10-13 weeks. It involves taking a small sample of cells from the placenta to test for chromosomal abnormalities.
- Amniocentesis: Usually performed after 15 weeks. It involves taking a small sample of the amniotic fluid surrounding the baby.
Both CVS and amniocentesis are diagnostic tests with a near-100% accuracy rate for detecting chromosomal conditions, but they do carry a small risk of miscarriage (typically cited as less than 1%).
What Are the Risks of an NT Scan?
This is one of the most reassuring aspects of the NT scan: there are no known risks to you or your baby. It is a non-invasive ultrasound that uses sound waves, not radiation. It is considered an extremely safe procedure for both mother and baby.
Does the NT Scan Hurt?
No, the NT scan is not painful. You will feel the cool sensation of the ultrasound gel and the gentle pressure of the transducer moving across your abdomen, but it should not cause any pain. If a transvaginal scan is required, you might feel some slight discomfort or pressure, but it is generally well-tolerated and brief.
Schedule your comfortable and pain-free NT scan with your healthcare provider to get your first detailed look at your little one.
At What NT Measurement Is There a Risk of Down Syndrome?
While there is no single “cut-off” number that guarantees a condition, measurements are assessed on a continuum:
- Below 2.5mm: Generally considered within the normal range and associated with a lower risk.
- 2.5mm – 3.5mm: A borderline or increased measurement. The risk is calculated by combining this measurement with your age and blood test results.
- Above 3.5mm (or >3.0mm in some guidelines): Considered significantly increased and is associated with a higher probability of chromosomal abnormalities, as well as potential heart defects.
It is essential to reiterate that the measurement alone is not diagnostic. A baby with a large NT measurement can be perfectly healthy, and the measurement will be factored into your overall combined screening result.
Factors Used to Determine Risk of Abnormalities
The final risk assessment from the combined screening is a sophisticated calculation that integrates several pieces of information:
- The NT Measurement: The precise millimeter measurement.
- Maternal Age: The baseline risk for chromosomal conditions increases with maternal age.
- Gestational Age: The exact age of the baby at the time of the scan.
- Blood Test Results: The levels of PAPP-A and hCG in your blood.
- Nasal Bone: The sonographer will also check for the presence or absence of the fetal nasal bone, as an absent nasal bone can be a soft marker for Down syndrome.
A computer program analyzes all this data to generate your personalized risk ratio.

10 Frequently Asked Questions (FAQ) About the Nuchal Fold Scan
1. Is the NT scan mandatory?
No, it is an optional screening test. The decision to have it is a personal one, and you should discuss the pros and cons with your healthcare provider.
2. How accurate is the NT scan?
When combined with the first-trimester blood tests, it can detect about 85-90% of babies with Down syndrome, with a 5% false-positive rate.
3. Can the NT scan detect the baby’s gender?
It is usually too early to determine gender reliably via an NT scan. This is typically done at the 20-week anatomy scan.
4. What if my baby is in a bad position during the scan?
The sonographer may ask you to cough, change position, or take a short walk to encourage the baby to move. Sometimes, a follow-up appointment may be needed.
5. Does a low-risk result guarantee a healthy baby?
No. A low-risk result significantly reduces the chance of the specific conditions screened for (Trisomy 21, 18, 13), but it cannot rule out all possible birth defects or genetic conditions.
6. Can the scan detect twins?
Yes, and it is particularly important in twin pregnancies. Each baby will have their own NT measurement taken.
7. What other conditions can a large NT indicate?
Besides chromosomal issues, a large NT can sometimes be associated with congenital heart defects and other rare genetic syndromes.
8. Should I have the NT scan if I’m young and healthy?
Yes, because while the baseline risk is lower, chromosomal abnormalities can occur in pregnancies of women of all ages.
9. What’s the difference between the NT scan and the NIPT?
The Non-Invasive Prenatal Test (NIPT) is a blood test that analyzes fetal DNA in the mother’s blood. It is a more accurate screening test for common chromosomal conditions but is often more expensive. Many women choose to have both, or their doctor may recommend one over the other based on their situation.
10. Where can I get an NT scan?
It is typically performed at specialized prenatal diagnostic centers or maternal-fetal medicine departments by certified sonographers and doctors.
Ready to talk it over? Your healthcare provider can help you understand your options and put your mind at ease. Book your appointment now!
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. Always consult with your qualified healthcare provider or a genetic counselor to discuss your individual circumstances, test results, and any concerns you may have about your pregnancy.
